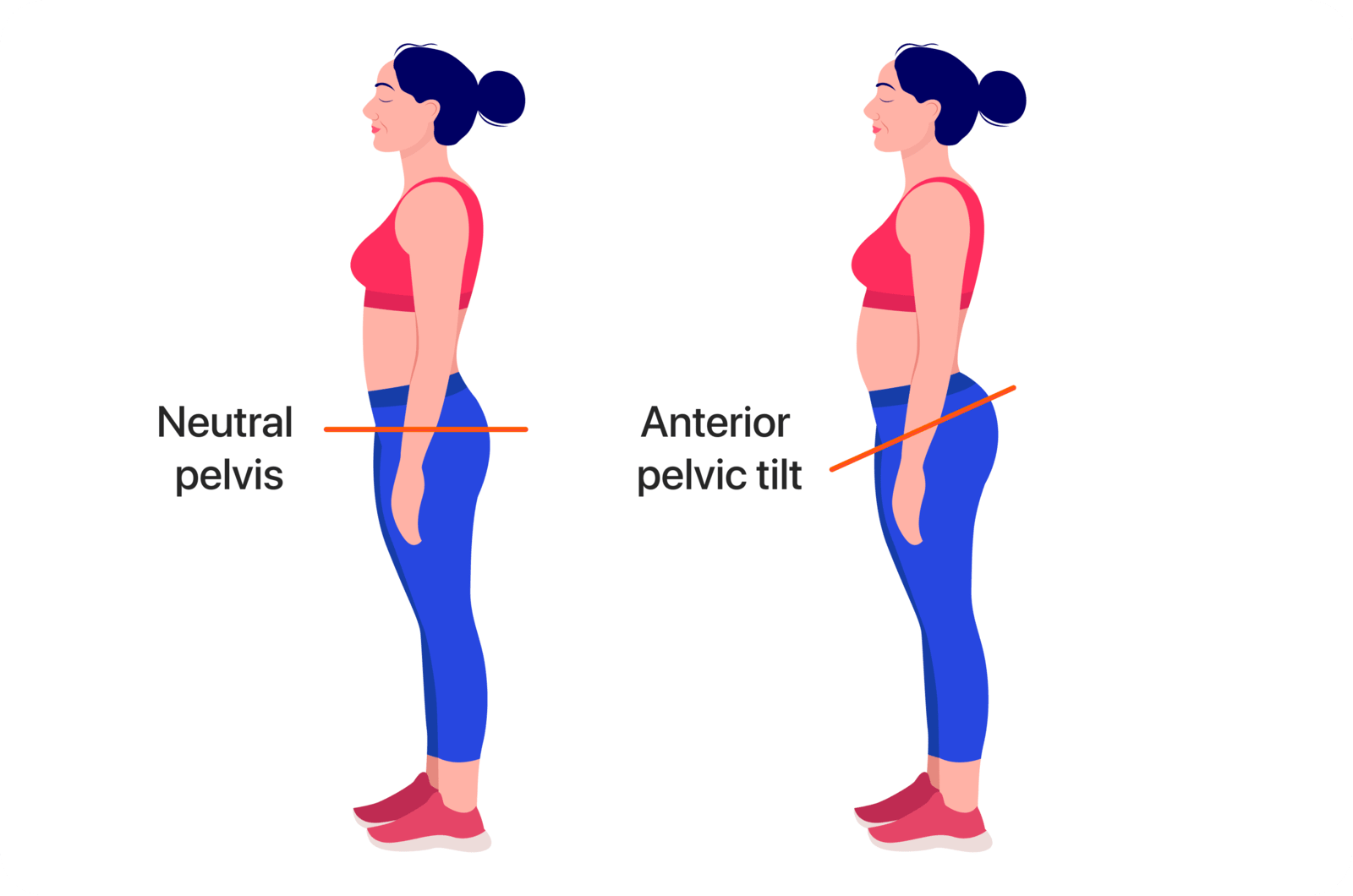
Understanding Anterior Pelvic Tilt (APT) and Hyperlordosis:
Anterior Pelvic Tilt (APT) is a postural deviation characterized by an increased forward tilt of the
pelvis, often accompanied by exaggerated lumbar lordosis. Here’s an overview with specialized terminology:
1.Pelvic and Spinal Kinematics:
• APT involves an increased anterior tilt of the pelvic area, it is typically
associated with an exaggerated lumbar lordotic curve and a forward-shifted center of gravity.
• This alignment can change the normal biomechanics of the lumbo-pelvic-hip complex,
affecting spinal loading and lower limb mechanics.
2.Musculoskeletal Imbalances:
• APT is commonly linked with shortened and hypertonic hip flexors (like the iliopsoas
and rectus femoris) and lumbar extensors.
• There’s often concurrent weakness or inhibition of the abdominal musculature
(particularly the transversus abdominis and internal obliques) and the gluteal muscles.
3.Functional Consequences:
• APT can lead to compensatory postural changes, potentially causing lower back pain
and altering lower extremity biomechanics, which impacts activities such as walking and running.
Advanced analysis and Assessment Strategies for APT:
1.Postural Analysis:
• Examine static posture thoroughly to determine pelvic tilt angle, lumbar lordosis,
and general spinal alignment.
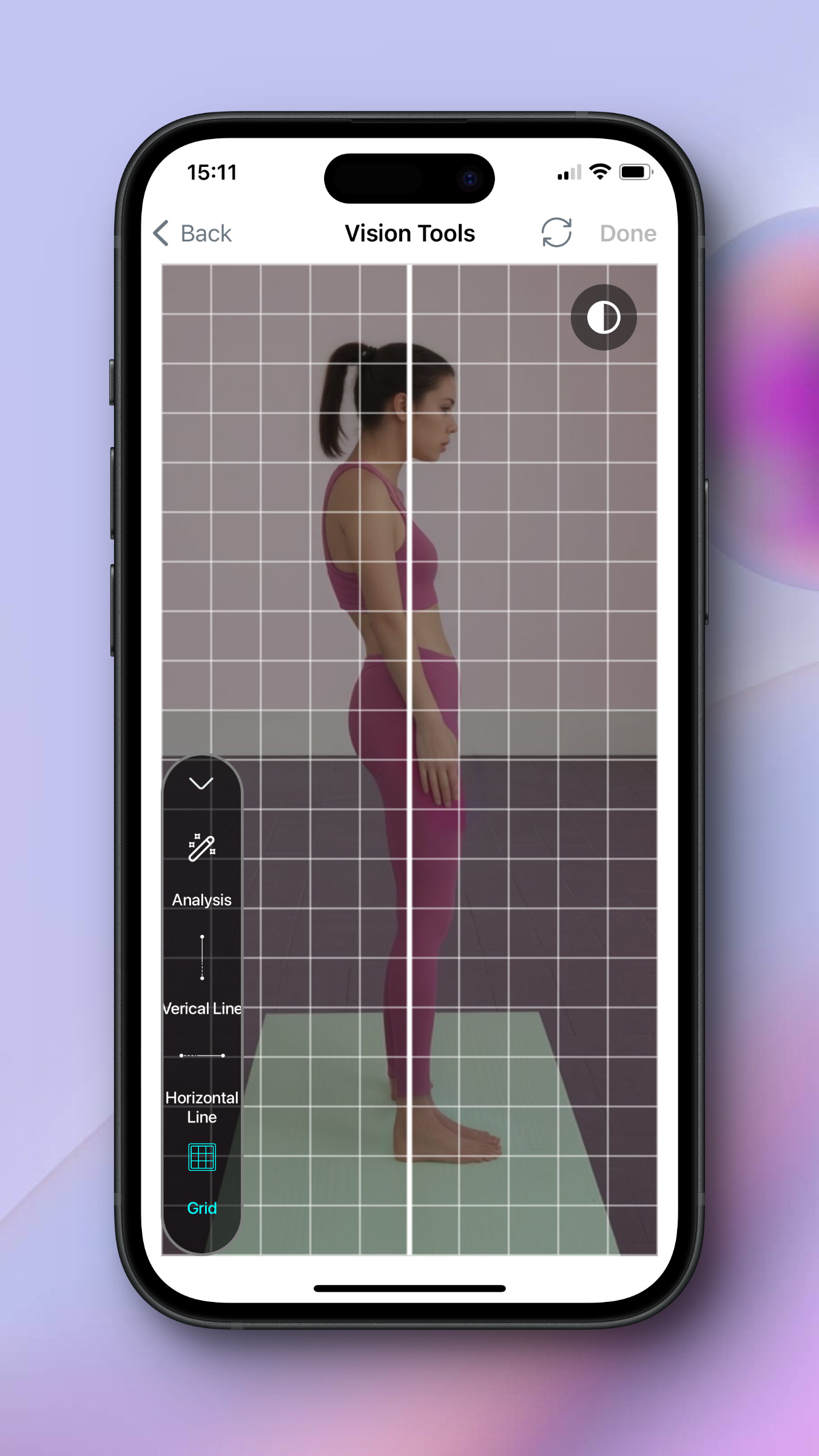
• Utilize tools such as plumb line assessments or postural analysis software for
accurate measurements.
2.Muscle Function Testing:
• Perform assessments of muscle strength and flexibility, particularly focusing on the
hip flexors, extensors, and core stabilizers.
• Manual muscle testing and the use of flexitrace applications or goniometers for joint
range of motion assessment are both effective.
3.Gait and Movement Analysis:
• Carry out a biomechanical evaluation of gait patterns and functional movements to
determine how APT affects dynamic postures. This can provide insights into compensatory mechanisms and
guide targeted interventions.
Analysing Knock Knees, Here's a step-by-step guide:
1.Activities and Medical History
With access to the Patient History and Symptoms Review: such as knee discomfort, instability, or trouble
performing specific motions Assess how everyday activities, sports, or occupational demands may affect or
aggravate the issue, as well as any history of knee injuries, surgeries, or underlying disorders such as
arthritis.
2.Postural Analysis and Visual Inspection:
• Static Analysis: Assess knee alignment by observing the patient's standing position.
• Dynamic Analysis: Monitor the patient's functional motions.
3.Functional Movement Assessment:
• Gait Analysis: Examine your walking patterns for any indications of knee valgus.
Specific Tests: Perform functional tests such as single-leg squats or step-downs to assess knee alignment
and lunges.
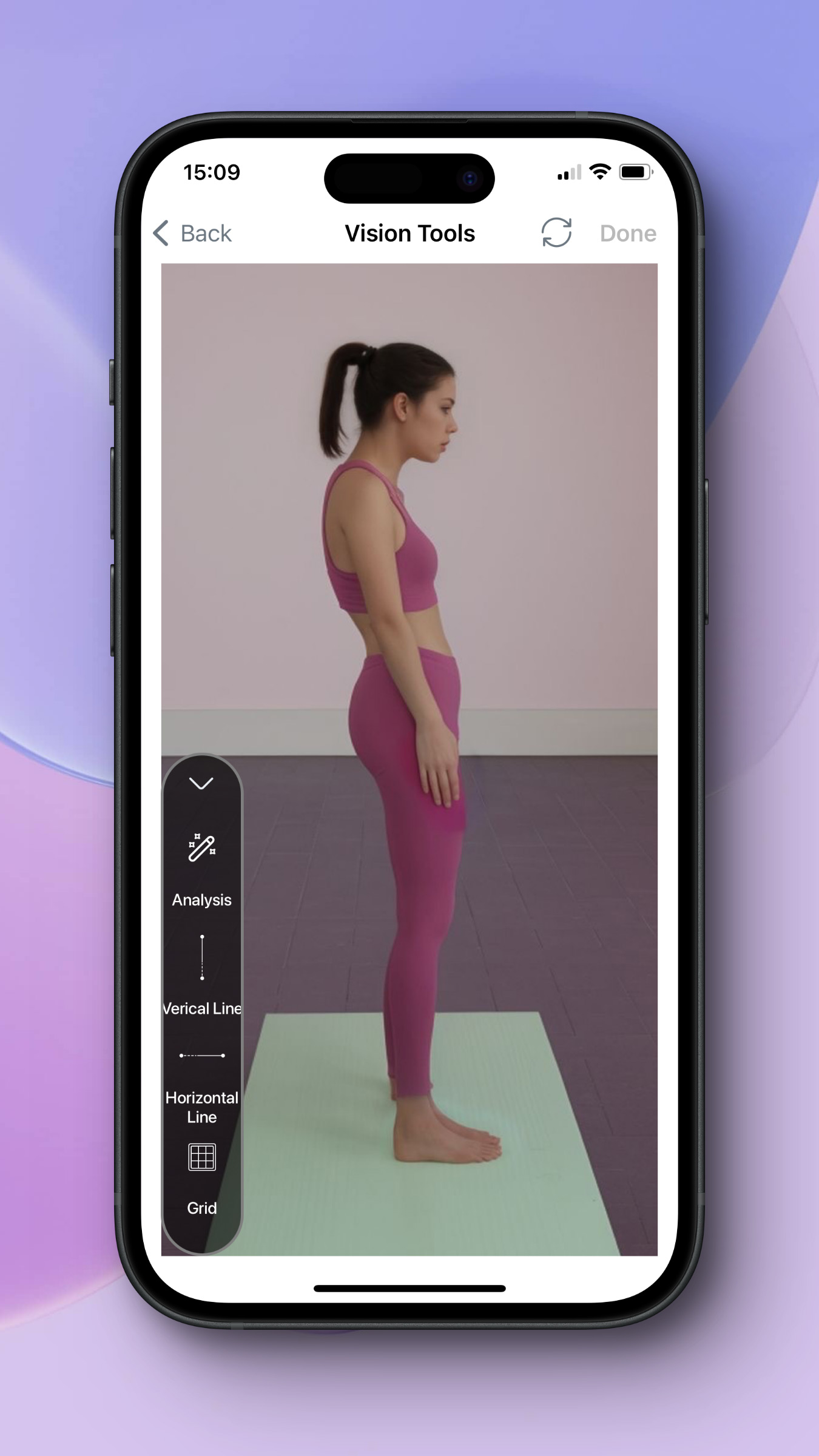
Choose postural analysis and upload a photo or take a picture of your subject.
Select the analysis and see the result from joint detection and alignments.
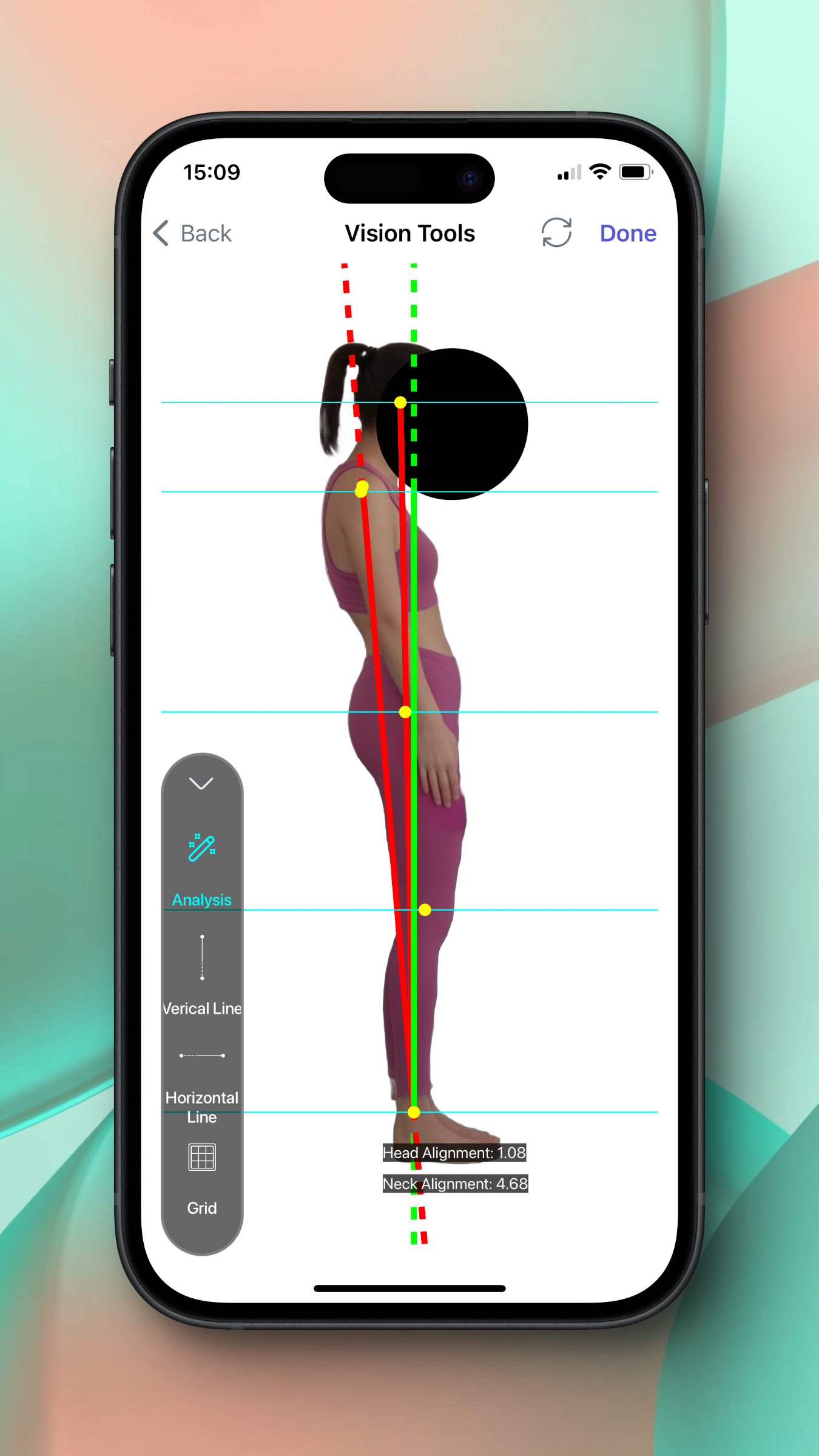
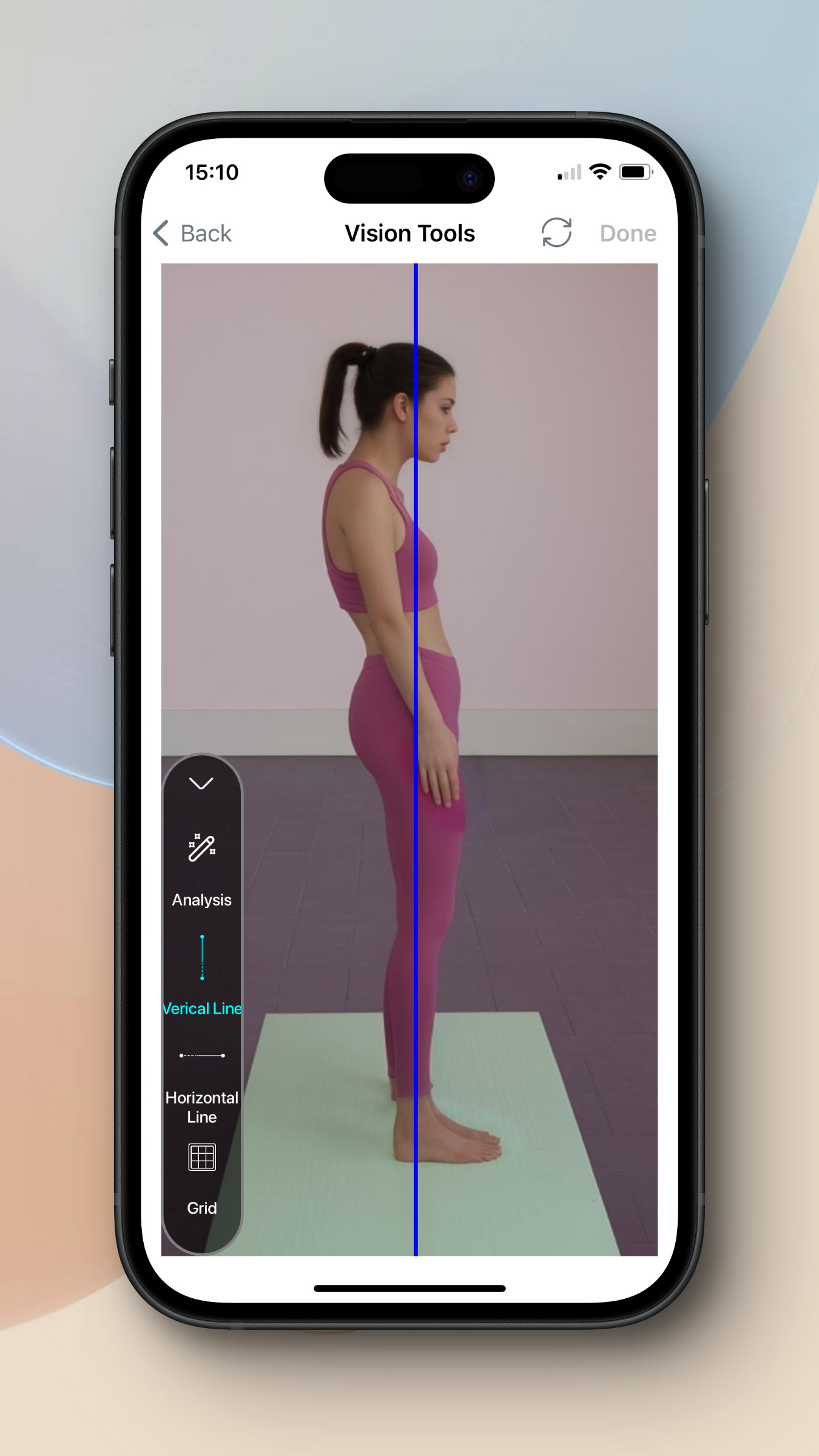
For more details use a vertical line on the ankle and knee and another on the axis, if your subject has APT, both lines will have differences.
For more details add grid. After assessing with our application you can record and save the process of therapeutic exercise.

Engage core, back straight, arms locked, squeeze glutes and hold for 15-20 seconds..

Lie down, knees bent, lift hips, squeeze shoulder blades, hold 15 seconds, repeat 10 times.

On forearms, tuck toes under, lift hips up, engage core, hold for 30-60 seconds.
There is an essential difference between APT and hyperlordosis; each might be the cause of the other and
dynamic testing is required for accurate analysis
Interventional Strategies:
1.Targeted Exercise Therapy for APT and Hyperlordosis:
• ATP-targeted exercises include hip flexor stretches and strengthening the glutes and
core muscles to restore a balanced pelvic position. Hyperlordosis exercises focusing on strengthening the
abdominal muscles and stretching the hip flexors can help correct the posture and reduce the excessive
arching of the lower back.
• Integrate core stabilization exercises like planks, Glutes Bridge, and cat camel
stretch to enhance lumber-pelvic control, vital for lifting techniques and sports performance.
2.Manual Therapy and Mobilizations:
• Utilize soft tissue mobilization, myofascial release, and joint mobilizations to
address musculoskeletal restrictions. This can be particularly effective in relieving tension and
improving mobility in athletes and fitness enthusiasts.
3.Neuromuscular Re-education and Ergonomic Training:
• Focus on proprioceptive training, such as balance and stability exercises, to promote
optimal pelvic alignment and movement patterns. This is essential for athletes to maintain balance and
coordination during dynamic movements.
• Advise on ergonomic adjustments in daily and sports-related activities to minimize
compensatory strains, crucial for maintaining proper posture and alignment during workouts and in
competitive environments.
Conclusion
Anterior Pelvic Tilt (APT) involves a forward tilt of the pelvis, causing an exaggerated lower back curve,
often leading to pain and mobility issues. Lifestyle factors like prolonged sitting contribute to APT,
impacting muscle balance and function. assessments involve analyzing posture, muscle strength, and
movement patterns, while intervention strategies focus on targeted exercises, manual therapy, and
ergonomic adjustments to correct alignment and improve mobility. Early detection and comprehensive care
are key for managing APT and its related condition, hyperlordosis. Dynamic testing is crucial for accurate
analysis and tracking progress in treatment.
| All Rights Reserved | FlexiTrace Developers LTD